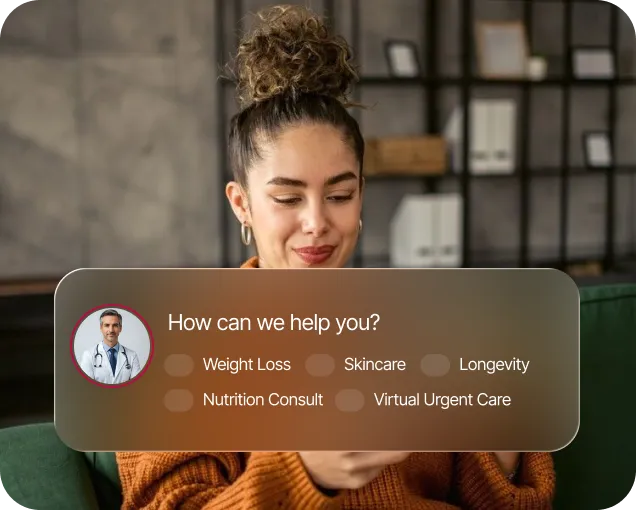
100% online process
No membership requirements
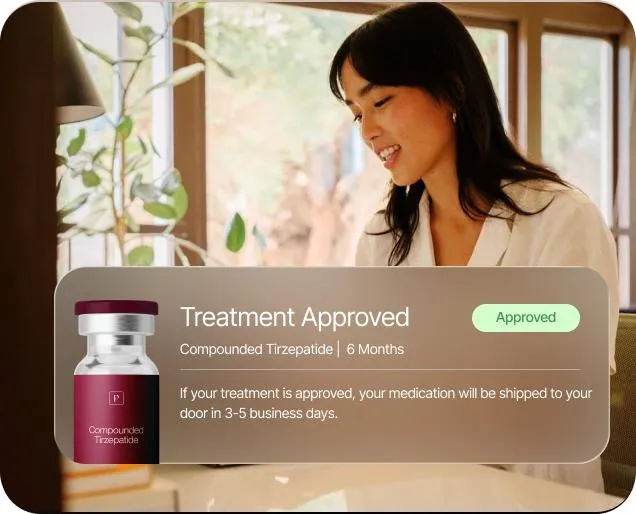
FDA-Regulated Pharmacies
Transparent pricing, no hidden fees
3-5 Business Days Turnaround Time
Trusted By 100,000+ patients
100% online process
No membership requirements
FDA-Regulated Pharmacies
Transparent pricing, no hidden fees
3-5 Business Days Turnaround Time
Trusted By 100,000+ patients




.webp)